Electronic health records (EHR) are an important solution that almost all medical organizations have adopted as part of digital transformation.
For instance, adoption rates for basic EHR functionality are 96% for hospitals and 78% for office-based physicians US-wide, according to Office of the National Coordinator (ONC).
Still, having an EHR system is a first step in increasing a hospital’s capacity. Software must be well adapted to solve ongoing and emerging challenges.
To solve the challenges of adopting and adjusting an EHR system, an organization might need experts in healthcare software development and maintenance who will help with the system’s safety, integrity, and feature delivery.
Yet, understanding the technical side of implementing an EHR system is important for efficiency. Therefore, let’s check out EHR software development in detail.
1
What is EHR Software?
An electronic health record (EHR) system is a digital platform that lets health organizations store and manage patients’ medical charts.
Typically, EHR systems help administer such information as:
- patient demographics
- medical histories
- immunization records
- diagnoses
- medication histories
- allergies
- laboratory test results
- treatment plans
- progress notes
EHR systems can streamline a clinic’s workflow by providing quick access to relevant patient information and test results. Also, they enable the sharing of patient information between all organizations involved in their care:
- laboratories
- family doctors
- pharmacies
- specializing clinics
- emergency facilities
- schools
etc.
EHRs facilitate medical decisions, help avoid delays in treatment, and reduce the probability of medical error.
Important barriers in the way to a successful EHR system implementation include:
- non-optimized processes
- staff resistance
- technical barriers
- lack of tech expertise
- legal hurdles
Here is why, for an efficient implementation, healthcare organizations should:
- evaluate their processes
- formulate requirements
- design an implementation plan
- cooperate with an experienced IT service provider
- adjust internal processes
- provide staff training and check feedback
- continuously monitor regulation compliance
What is the Difference between EHR and EMR?
You use EHR to exchange patient information with others and EMR to keep your records in good order.
The difference between an electronic health record (EHR) and an electronic medical record (EMR) lies in interoperability.
An EHR, which contains data from multiple sources, has been designed for comprehensive data sharing, while an EMR is used internally within a single practice.
As a result, an EHR provides a wide scope of information, and an EMR offers a narrow focus on diagnostics, treatment, and disease progression.
Another key difference is that an EHR system allows patients to access health and treatment information, while an EMR system does not.
2
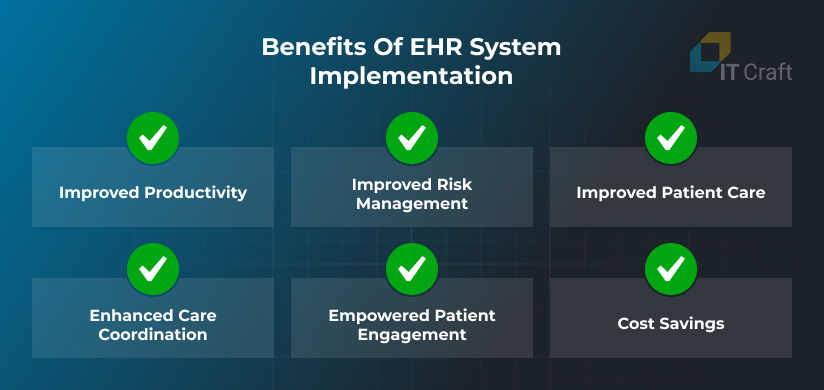
Benefits of EHR System Implementation
An EHR system improves the quality, efficiency, and safety of provided services. It lets health organizations go beyond the standard data collection in their offices without constantly requesting other health organizations.
Your organization can expect further benefits from integrating an EHR system:
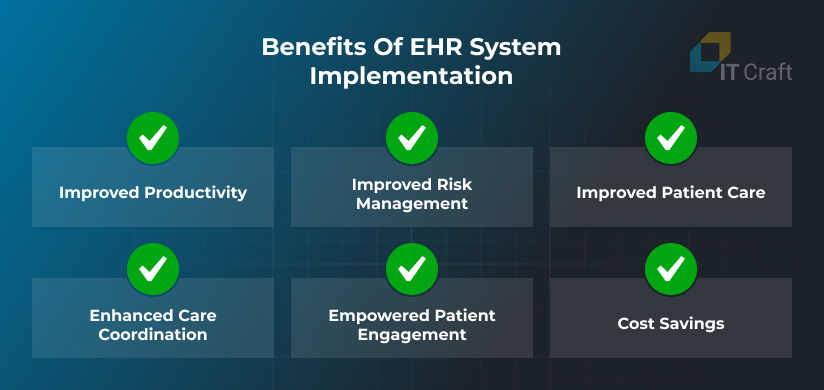
Improved Productivity
An EHR system decreases administrative workload by requiring less time to search and retrieve relevant patient information, enabling doctors to spend more time on current patients or accept new patients.
Also, EHRs make all test results available, helping clinics save money on redundant testing.
Improved Risk Management
EHR systems are crucial for risk management. They store and manage comprehensive patient information, including medical history, treatment and medication plans, test results, allergies, and more, helping with a well-weighted medical decision.
At the same time, EHR systems help expose safety problems, prevent adverse events, and decrease probability of medical error.
Improved Patient Care
Besides tracking accurate patient records and making informed decisions, EHR systems can help identify and address operational issues.
Patient convenience also increases. For instance, e-prescription functionality simplifies the process of obtaining medications. In addition, EHRs can improve the accuracy of diagnostic coding and billing.
Enhanced Care Coordination
EHRs streamline information exchange between different healthcare organizations or departments within one organization, turning disconnected doctors’ interactions with a patient into one big picture.
More importantly, EHR systems can buy time when identifying a relevant emergency treatment, ensuring unrelated but important conditions are noticed quickly.
Empowered Patient Engagement
Patients can access diagnoses, useful treatment information, self-care instructions, and reminders via connected patient portals or mobile apps. They can also use EHR self-service functionality to manage appointments or report symptoms.
Subscribing e-referrals simplifies follow-up care with narrow-focused specialists.
Cost Savings
The above enhancements decrease the waste of valuable hospital time and resources, translating into cost savings.
Moreover, while EHR solutions help with accurate and timely billing and diagnosis coding, the number of claims and charge denials decreases. The system can also alert when a test or treatment can be applied only at a certain frequency.
3
EHR Software Development Technologies
Security is critical when selecting a technology for custom EHR software development. The source code must meet stringent quality criteria, ensuring patient data is safe and secure.
The project team should prefer a framework (Laravel, Node.js, and similar technologies) over a CMS (Drupal, WordPress, and similar technologies). A CMS can make it difficult to reach the required security level.
Otherwise, technological stack can vary flexibly from one EHR software development project to another, depending on a project team’s expertise and preferences.
Developers can use the following technologies for different parts of custom EHR software development:

Front end
These technologies are used to build the visual part of web-based software.
Mobile
Developers can use native languages to build two separate apps for each specific platform or use cross-platform frameworks to produce two apps within one codebase.
Back end
The back end is responsible for data collection, processing, and exchange; therefore, it must be robust, flexible, and secure.
Databases
Developers often need to integrate several databases for different data types to ensure best software performance. The focus remains on database security and integrity.
Search
It is used to boost search through topics, messages, health records, and more.
Payment processing
The team should integrate a certified processor to ensure secure payments.
Telehealth and communication
Developers can integrate several services for in-app messaging, video and voice calls, SIP calls, emails, and messenger chats.
Security
The team must implement enhanced security mechanisms to protect sensitive data.
Deployment
Containerization is used to increase software resilience and scalability in the cloud.
Cloud
By developing a cloud solution and optimizing infrastructure consumption according to client needs, the project team can ship new updates and features quickly and efficiently.
Testing
These testing tools help automate different testing activities, saving hours of manual work on a development project.
AI
AI technologies let healthcare organizations leverage accumulated data, boosting analytics, insights, diagnostics improvement, security, and more.
Team collaboration
The team uses these tools to improve communication and harmonize efforts on a project.
4
Key Features and Requirements of an EHR System
The top reason for implementing an EHR system is to support growth. Organizations want to receive greater functionality that improves process efficiency.
Let’s discuss what functionality and related requirements a healthcare organization could include in an EHR system implementation to meet growing needs:

Practice Management
Practice management provides the functionality and access to data needed for: completing administrative tasks, such as
- schedule management,
- workload and cost tracking,
- customer management,
- compliance monitoring,
and more.
A dynamic dashboard is the central part of practice management. Administrators can use it to group functionality, customize information, and manage feature complexity.
Digital Intake
Digital intake functionality optimizes data administration, eliminating the need for multiple data reentries. Clinic administrators can also easily correct and expand the required entries.
It is also important that the EHR system can receive and process data from external sources, enabling document upload and image recognition.
Electronic Health Records
Electronic health records (EHRs) are the key feature of an EHR system. They simplify entering, storing, and updating patients’ clinical information.
Realization can vary between various providers, offering different degrees of customization and integration.
Specialized facilities require niche functionality to best support the needs of SUD treatment, residential/inpatient programs, agencies involved in autism/IDD care, and more.
Patient Engagement
An EHR system can include a web-based patient portal or a mobile app to improve patients’ access to related treatment information and medical documentation.
Treatment coordination also improves while patients receive notifications on upcoming tests and procedures. Self-scheduling functionality lets them manage appointments, decreasing no-show rates.
Message/Email Manager
Message/Email manager functionality can be launched as part of a patient portal or a stand-alone module and is used for sending secure notifications about upcoming appointments, tests, return visits, and more.
Message/Email managers can replace paper-based correspondence between healthcare providers, patients, and insurance companies, serving secure release and exchange of sensitive medical information.
Telehealth/Virtual Visits
Telehealth is a booming trend. Its market size is estimated at $151M and is expected to grow to $290 by 2028.
Telehealth functionality helps decrease the number of in-person visits where applicable.
It can provide audio and video calls, live chat, and screen sharing to ensure efficient communication between patients and healthcare professionals.
Billing
Billing is one of the key modules for healthcare organizations of all sizes, with special emphasis on revenue cycle management. It lets organizations monitor revenue streams and address emerging problems proactively.
Important billing functionality includes:
- quick insurance validation,
- treatment coding verification,
- invoice tracking,
- support of different payment methods, and
- claim management
Reports and Analytics
EHR software can generate standard reports and provide customization functionality when an organization needs to focus on specific aspects of patient care quality and outcomes.
Reports and analytics can also include maintenance, updates, and submission to designated recipients. Guidelines on report creation help decrease training time.
AI Functionality
AI is applied to a growing range of tasks, including:
- automation of administrative activities (e.g., find and remove duplicates)
- test recognition and diagnostics support
- turning conversations between doctors and patients into documentation
- improving search through available data
and more.
Also, patients can use conversational chatbots to search for information or schedule an appointment.
Do you have a vision of AI functionality in your mind?
Let’s discuss it and estimate possible implementation costs. It’s free!
Contact Us
Integrations
Ease of integration is one of the main requirements of an EHR system. Healthcare organizations can exchange data seamlessly with laboratories, clinics, and primary care providers using APIs, which connect with their systems.
Prescription management is essential for both patient convenience and improved control over-prescribed medication, which also requires API development.
Marketing Automation
Marketing functionality can be implemented as part of patient portal or messaging functionality to help clinics notify patients of useful services or special events.
Also, patient satisfaction surveys and feedback forms can help organizations evaluate performance and identify improvement areas.
5
Types of EHR Software
The type of EHR software can affect development and implementation strategy. You can choose among the following types of EHR software, each having specific benefits and limitations:
Off-the-Shelf vs. Custom-Built
Off-the-shelf means buying a software license or a subscription for ready-made solution by a certified provider, and it can be a nice option for starting digital transformation. Still, everything extra, e.g., seamless data exchange, may require customization work.
A custom solution is an alternative for organizations that understand their digital needs and want to adjust software to those needs as much as possible. However, upfront costs can be high.
On-Premises vs. Cloud
On-premises means an organization buys and installs servers internally to store and process patient data. Large initial investment can be required, as well as regular server updates and maintenance, but data control improves.
Cloud means hosting data online at third-party vendors that help with maintenance and updates. Initial costs are low, and the organization pays for its computing time. Still, monitoring and occasional audits are required to ensure optimized cloud infrastructure usage.
General vs. Specialized
EHR systems vary to meet the needs of different healthcare professionals. There are systems for general clinics and practices.
However, niche practices like plastic surgery, skincare, or mental health may find general software impractical. They can look for a specialized EHR system adjusted to their unique workflows.
6
How to Build an EHR System
EHR system development and integration is a complex process that requires:
- careful assessment of an organization’s implemented software system and improvement areas
- constant focus on value delivery during project development
- enhanced security of software source code and infrastructure
- conformity to applied regulations on sensitive data storage and processing
Here are essential steps on an EHR project that let both receive immediate positive changes and reach long-term transformations:

Audit of Implemented System and Related Processes
Because healthcare organizations already have software in use, the development team must audit the implemented software to:
- determine flaws and improvement areas in current processes,
- think of applicable standards and regulations it must meet, and
- analyze technical and user-related risks
Also, the project team needs to consider integrating the new software with the required internal and external solutions.
Determine New System Requirements
Software developers actively interview system users and stakeholders to collect missing or unaccounted requirements. Key points include:
- system users and their roles,
- user goals, tasks, and accesses to patient data, and
- expectations from the new system
The project manager discusses identified requirements with stakeholders to ensure an aligned vision of the future system.
Deciding on Specific Solution
Here, the team chooses an implementation path that meets the client’s goals and limitations. Based on the audit and requirements, the team can decide on:
- selecting, customizing, and integrating an available third-party solution
- delivering a custom-built product from scratch
Also, the team can reuse some existing source code or decide to replace it with a new system gradually.
EHR Software Development and Implementation
The project team ships new software functionality in fast-paced Sprints, which allows them to receive immediate stakeholders’ feedback and elaborate quickly, which is needed to evade the risks of a major project rework.
The team completes the following activities throughout a Sprint:
- front-end, back-end, and mobile development,
- QA and testing to meet quality standards and project requirements,
- feature deployment
- integration with required external and internal software
- User Acceptance Testing (UAT) by stakeholders
- feedback incorporations to ensure expectations are met
Maintenance, Updates, and Expansion
Assigned specialists monitor system integrity and security of software infrastructure to detect system slowdown, cyber threats, or unreasonable resource consumption.
Also, the project team must regularly update the source code to close vulnerabilities, ensure conformity to new regulations, and meet evolving user needs.
Do you need help optimizing resource consumption?
Let’s start with an audit and identify areas where you could pay less for more.
Contact Us
7
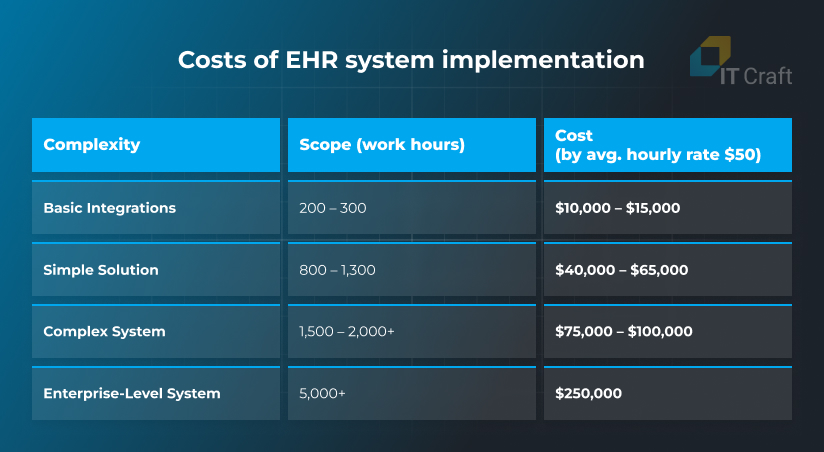
Costs of EHR Software Development and Integration
Upfront costs of EHR implementation vary between $10,000 and $250,000+, depending on complexity of provided requirements and a vendor’s hourly rate.
Basic Integrations
You invest time and money into integrating existing EHR software into your processes, ensuring secure, flawless, and well-adjusted data flow.
You may require EHR customization, help with infrastructure deployment, its optimization in a certified cloud, or API integrations to automate data exchange and improve billing.
Basic integrations require 200 – 300 work hours, costing you $10,000 – $15,000.
Simple Solution
A simple solution can be a module or a stand-alone app aimed at completing one straightforward operation. It has only key functionality and minimum customization.
An example of a simple solution can be a patient intake form or patient engagement functionality, which can be implemented as a responsive web solution. Web implementation makes the functionality available from all devices for minimal investment.
A simple system requires 800 – 1,300 work hours to complete. The costs start at $40,000 – $65,000.
Complex System
A complex system contains a rich feature list and optimized workflow. It also has a modular structure that lets customize and expand the system flexibly per changing needs.
In addition to EHR management, the team can develop or integrate telemedicine functionality, advanced reports and analytics, patient notifications, billing and payment processing, and more.
A complex project timeline involves 1,500 – 2,000+ work hours, and required costs start at $75,000 – $100,000.
Enterprise-Level System
An enterprise-level system meets the needs of large organizations. It contains sophisticated business logic, large data storage, heavy back-end calculations, and multiple seamless integrations with third-party services.
Additional features can include AI integrations, a custom API, administration panel, data analysis and custom reports, and more. It has the highest security level and complies with local and international regulations.
An enterprise-level system can take 5,000+ work hours to build and deliver, and required costs start at $250,000 and higher.
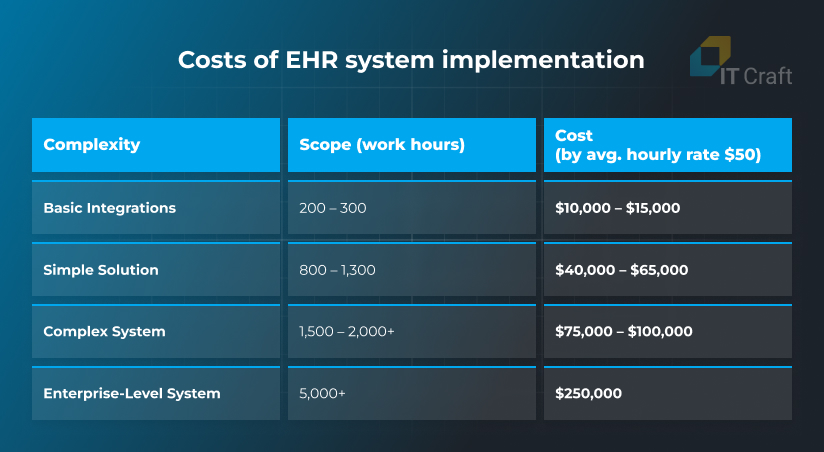
Maintenance costs
Remember to factor in maintenance and update costs. The allocated budget depends on software size and complexity, requiring 15%–20% of initial development costs per year.
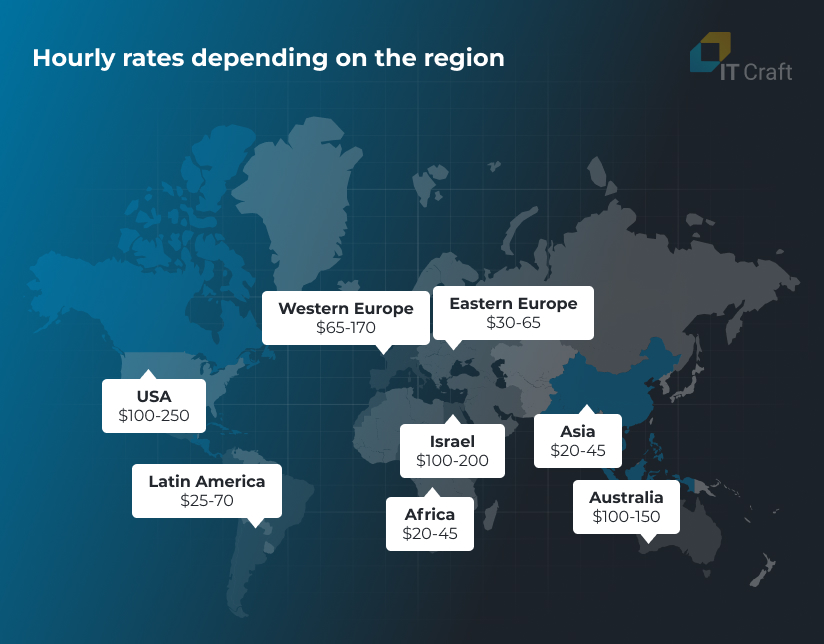
Hourly rates
Software development prices depend on the cost of living in a region, which is why certain areas provide competitive pricing. However, cultural and communication barriers can be high.
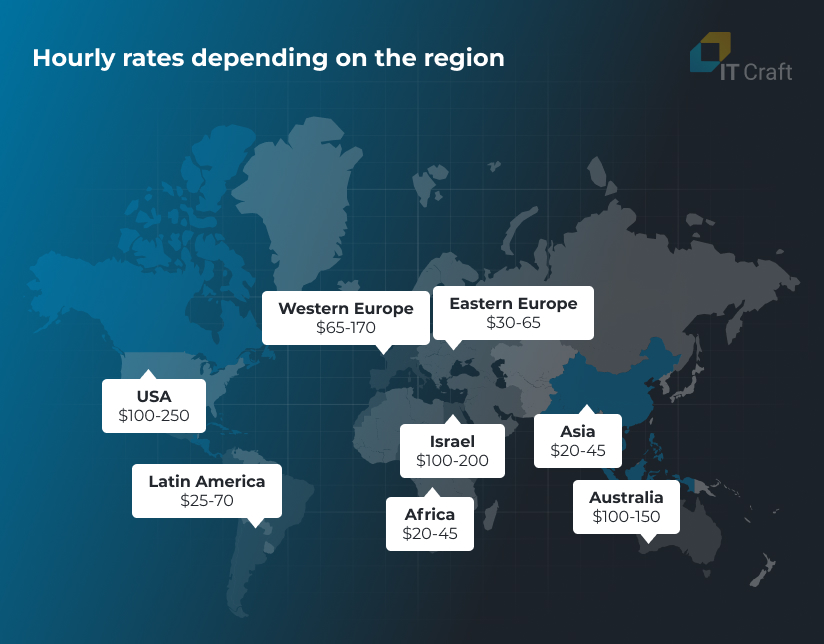
An important note: A development service provider usually calculates the costs of EHR software development within a range, and due to project complexity, we recommend sticking to the high end of that range.
Are you looking for the best value for your budget?
Schedule an introduction call with our HealthTech team to discuss how our custom EHR software development services could meet your project needs.
Contact Us
8
EHR Software Development with IT Craft
IT Craft engineers can help you at any step of EHR software development and maintenance, including:
- project discovery
- web and mobile development from scratch
- IT consulting and audit
- software modernization
- solution expansion
- infrastructure optimization and scaling
and more.
As a reliable, long-term partner for healthcare startups and established organizations, IT Craft provides flexible services to meet changing development needs.
You can:
- hire a dedicated team that becomes your external IT department,
- choose IT staff augmentation to extend your tech team with narrow expertise or
- apply to managed services to ensure your system is secure, scalable, and optimized
Arctrieval Legal
This project started as a secure system for medical correspondence and release of patient information and later morphed into a solution for managing medical and billing record requests.
The client needed
The client initially wanted to replace cumbersome paper-based processes with a reliable cloud-based system, allowing consumers and authorized third parties to retrieve medical information quickly.
How we helped
IT Craft developers started with an audit of available source code and offered an alternative solution that enabled the client to improve security and scalability. The IT Craft team later assisted in project updates and further pivot to help the client efficiently deliver a new product to the market.

!
Summary
EHR software development enables healthcare organizations to build a system for their needs and adapt it as soon as those change.
Careful implementation is worth the effort because it decreases workload, improves process transparency, reduces staff burnout, increases patient satisfaction, and enhances revenues.
It is important to turn to domain experts who can help identify feature and system requirements, design a flexible architecture, and set up secure software infrastructure to launch a solution that meets high standards.